Case-Based
Learning in Family Medicine
Musculoskeletal Medicine/Office Orthopedics
Wm. MacMillan
Rodney, M.D.
April 28, 1994 (Updated 1994, 1996, 1998, 1999)
|
|
Edited and Abridged from
Schultz RJ. The Language of Fractures, 1st
Edition. Williams and Wilkins, Baltimore, MD, 1972.
I. ESSENTIAL FRACTURE DEFINITIONS
A. A fracture is a complete
or incomplete break in the continuity of bone or cartilage.
B. A complete fracture is
one where both cortices of the bone have been broken as opposed to an
incomplete fracture where only one cortex has been broken. See V.F. for examples of incomplete
fractures (Greenstick and Torus).
If a fracture contains
more than two fragments, it is classified as a comminuted fracture.
D. A comminuted fracture may have three or more pieces with various directional orientations. Simply refer to the entire collection of pieces as comminuted. A comminuted fracture is one that has more than two fracture fragments. This holds true whether the number is three or three thousand, regardless of location.
E. A closed or simple
fracture is one in which the skin and soft tissues overlying the fracture are
intact, and there is no communication with the outside environment.
F. An open or compound
fracture exists anytime the fracture site communicates with the outside
environment. This is true whether the
wound or skin defect is a small pin hole, puncture wound, or massive
disruption.
II. ESTABLISHING THE LOCATION OF FRACTURE
Reference
Points and How to Use Them
A. New fractures of the
shafts of long bones are said to be located in the proximal, middle, or distal
thirds or at their junctions (p. 11 attached).
B. Fractures at these
levels are referred to as fractures at the junction of the proximal and middle
third (PM3) and junction of the middle and distal third (MD3).
C. A lesion occurring at
about the midpoint of the bone, although located in the middle third, may be
referred to as a midshaft fracture.
III. DIRECTION OF FRACTURE LINES
A. Transverse fracture. A transverse
fracture is one that occurs when the fracture line is at right angles at the
cortices or long axis of the bone.
Transverse fractures may be complete or incomplete, open or closed, and
may occur at any location.
B. Oblique fracture. An
oblique fracture is one in which the fracture line runs obliquely to the long
axis of the bone or the cortices.
C. Spiral fracture. A spiral
fracture is caused by a torsional force and is somewhat like a long oblique
fracture that spans a greater area and encircles the shaft of the bone, thus
forming a spiral in relation to the long axis of the bone.

Reference: Schultz RJ. The Language of Fractures, 2nd Edition. Williams and Wilkins,
Baltimore, MD, 1990.
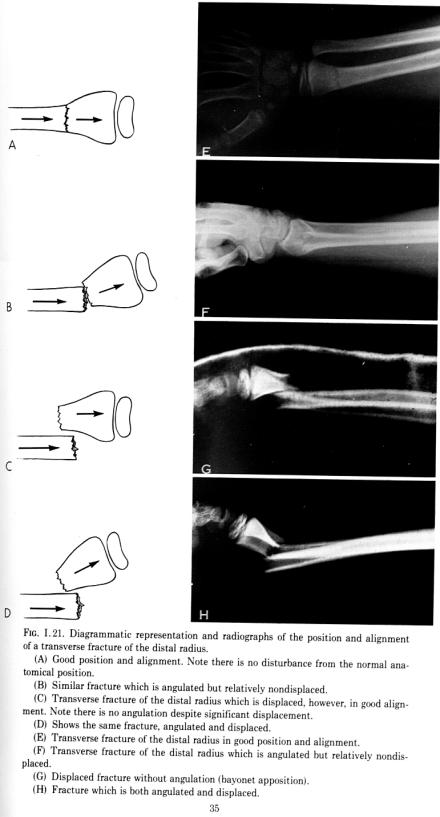
IV. POSITION: Alignment, Angulation, and Displacement
A. Alignment. Alignment is the
relationship of the longitudinal axis of one fragment to another. Deviation of alignment or mal-alignment is
the result of angulation of the fracture fragments.
B. Position. Position is the
relationship of the fragments to their normal anatomical structure. Loss of position is called displacement and
may result from the loss of apposition, over-riding, or rotation. In the shafts of long bones, various
combinations can occur.
“Bayonet apposition” is a displaced fracture without angulation
(see pp. 34, 35 attached).
C. Direction of angulation.
The description of the direction of angulation is often the source of
confusion. The direction of angulation
can be described by the following:
1. By the direction of
angular displacement of the distal fragment in relation to the proximal
fragment;
2. By the direction of the apex of the
angle formed by the fracture fragments.
Most often the direction of angulation is confused with the direction of angular displacement of the distal fragment. Too often, for example, a Colles’ fracture is said to have dorsal angulation when dorsal angular displacement of the distal fragment is meant. If the apex of the fractured radius is volar, this is called either volar angulation of the fracture or dorsal angular displacement of the distal fragment. Both methods are in common usage.
D. Displacement. Although
usage has obscured a precise meaning for displacement, displacement generally
signifies that the two fragments are no longer in contact.
V. OTHER DESCRIPTIVE TERMS
A. Distraction. Distraction
occurs when the opposing ends of the fracture fragments are kept apart. This may be the result of excessive traction
caused by the pull of tendons. This is
different from displacement.
B. Impaction. Impaction occurs
when one fragment of the bone is forcibly driven or telescoped into the
adjacent fragment or when the fracture fragments are allowed to press forcibly
against each other.
1.
Compression. A compression fracture of the vertebral body is a form of
impaction. This is a common fracture scene in our nursing home population.
2.
Impaction
fractures are also commonly seen in trauma.
C. Avulsion fractures. Violent
contraction of a muscle can cause rupture of the muscle belly or its tendon, or
can pull away a fragment of bone at the insertion of the tendon. At ligamentous insertions, violent trauma
applied in a direction, which places the ligament under great tension, may
avulse a fragment of bone, rather than rupture the ligament. Thus, an avulsion fracture occurs when
fragments of bone are pulled away from their original position. This is a form of “distraction.” (see V.A.)
D. Intraarticular fractures.
An intraarticular fracture is a fracture which extends into and involves
an articular surface of a joint. These
fractures may or may not be displaced.
Reference: Schultz RJ. The Language of Fractures, 1st Edition. Williams and
Wilkins, Baltimore, MD, 1972.
E. Stress fracture. A fatigue
or stress fracture is the result of repeated, relatively trivial, trauma to an
otherwise normal bone. It occurs not as
a sudden break, but as the result of alteration of the bone in the form of
gradual, local dissolution, secondary to repeated minor and usually
unaccustomed over use. This may or may
not result in a complete fracture.
Stress fractures occur most frequently in the lower extremities,
especially in the metatarsals.
F. Incomplete fractures.
Incomplete fractures occur when only one cortex of the bone has been
broken. Incomplete fractures are
relatively stable, and if protected, will tend maintain their position
indefinitely. Incomplete fractures are
common in the short bones, irregularly shaped bones, and flat bones. There are certain incomplete fractures which
occur exclusively in children, probably because of the elasticity of their
bones. These are greenstick fractures
and torus fractures.
a. Greenstick fracture. This
is an incomplete, angulated fracture producing bowing of the bone. It derives its name from its resemblance to
a young branch which, when broken, breaks on its outer surface, but is
maintained intact on its inner surface.
It should be noted that the broken cortex is always on the convex
aspect.
b.
Torus fracture. In contrast to a greenstick fracture, a torus fracture is an
incomplete fracture with a buckling of the cortex. Torus fractures are usually the result of compression forces and
may be considered a type of compression fracture or, in fact, and impaction for
x-ray.
VI. ADDITIONAL MISCELLANEOUS TERMS
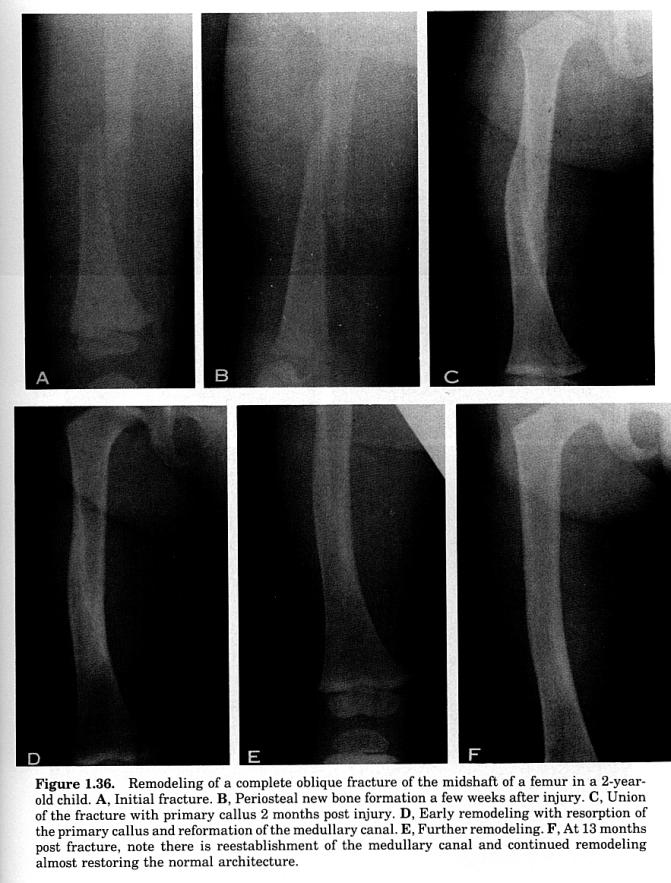
A. Remodeling Remodeling of a
complete oblique fracture of the midshaft of a femur in a 2-year-old
child. See Figure 1.36 next page.
1. Plate A. Initial fracture.
2. Plate B. Periosteal new bone formation in a few weeks after injury.
3. Plate C. Union of the fracture with
primary callus 2 months post injury.
4. Plate D. Early remodeling and
resorption of the primary callus.
5. Plate E. Further remodeling
6. Plate F. At 13 months post fracture, note there is re-establishment of the canal and continued remodeling almost restoring the normal architecture (see p. 55 attached).
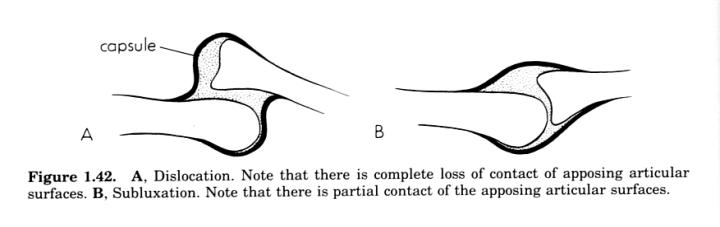
B. Dislocation. A dislocation
is a complete disruption of the joint with loss of contact between the articulating surfaces of adjacent
bones.
C. Subluxation. A subluxation
is a partial loss of continuity between the two opposing articular surfaces
with some part of the opposing articular surfaces remaining in contact. Subluxations may be very mild to very severe
(see p. 7 attached).
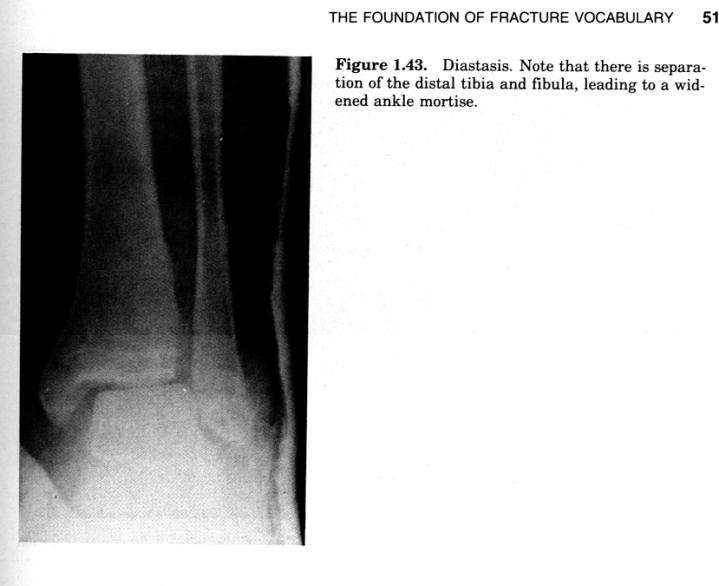
D. Diastasis. A diastasis is a
separation of normally joined parts, most commonly applied to slightly movable
joints. Diastases occur in the region
of the pubic symphysis or the distal tibiofibular syndesmosis (see p. 7
attached).
 Reference: Schultz RJ. The Language of Fractures, 2nd Edition. Williams and Wilkins,
Baltimore, MD, 1990.
Reference: Schultz RJ. The Language of Fractures, 2nd Edition. Williams and Wilkins,
Baltimore, MD, 1990.
 Reference:
Schultz RJ. The Language of Fractures, 2nd
Edition. Williams and Wilkins, Baltimore, MD, 1990.
Reference:
Schultz RJ. The Language of Fractures, 2nd
Edition. Williams and Wilkins, Baltimore, MD, 1990.
VII. REDUCTION OF FRACTURES
A. Closed reductions. Closed
reductions are reduction of fractures which do not require an operative
incision to be made. This type of
reduction is produced by traction or manipulation of the fractured fragments or
a combination of both.
B. Open reduction. Open
reduction is a restoration of the fracture fragments through surgical exposure
of the fractured site.
C. Fixation. Fixation is a
method of holding the fractured fragments into position following
reduction. Fixation may be performed by
external means such as cast immobilization or by internal means. (Casts are also placed in cases which do not
require reduction if one wants to be a purist--DPL.)
VIII. TERMS RELATED TO FRACTURE UNION
A. In delayed union, fracture repair, although retarded, is proceeding
and will eventually produce firm union just so long as additional adverse
stresses are not added.
B. Non-union exists when there is failure of union of the fracture
fragments and the processes of bone repair have ceased completely. With non-union, the opposing ends of the
fracture fragments become atrophic and the medullary canals have become covered
over by sclerotic, eburnated bone.
C. Slow union--there are many fractures that even under ideal
conditions are known to heal slowly.
Most importantly, slow union is not to be confused with delayed union,
which is retarded healing beyond the normal rate for a given fracture.
D. Mal-union. Mal-union occurs
when there is union of the fracture with angulatory for rotary deformity.
General Guidelines for Fractures that are Managed Operatively
(for
more specifics, see pp.12-14)
Edited and Abridged from Anderson BC.
Office Orthopedics for Primary Care Diagnosis and Treatment,
2nd Edition, 1999, ISBN
0-7216-7089-x
|
Fracture/Dislocation |
Reason
for Orthopedic Referral
|
Fractures that
require referral to orthopedic surgery
|
|
|
Multifragment
intra-articular |
Risk of arthritis
and malunion |
|
Fracture dislocations |
Difficulty of reduction, risk of arthritis |
|
Metastatic lesion of bone |
Risk of pathologic fracture |
|
Comminuted
fractures |
Risk of nonunion and angulation |
|
Compound fractures |
Risk of infectious
complication |
|
Fractures
associated with neurovascular compromise |
Soft-tissue injury |
General Guidelines for Fractures that are Managed
Nonoperatively
Fracture/Dislocation
|
Nonoperative immobilization or Treatment |
General
Categories of Fractures Managed Nonoperatively
|
|
|
All stress fractures |
Reduced running, standing, repetitious use |
|
All nondisplaced extra-articular fractures |
Casting for
3-6 weeks (WMR: or splinting equivalent)
|
|
Most small (flecks) avulsion fractures |
Casting for 2-4 weeks (WMR: or splinting equivalent) |
|
Some nondisplaced, single-fragment
intra-articular fractures |
Casting for 4-6 weeks (WMR: or splinting equivalent) |
HUMERUS
|
|
|
Fragment displacement <1cm or angulation
<450 |
Hanging cast plus pendulum stretching exercises |
CLAVICLE
|
|
|
Nonarticular proximal third |
Figure-of-eight splint or simple sling |
|
Middle third |
Figure-of-eight splint or simple sling |
|
Nondisplaced distal third |
Figure-of-eight splint or simple sling |
ELBOW
|
|
|
Dislocation without fracture |
Closed reduction with distal distraction |
|
Nondisplaced radial head fracture |
Simple sling and range-of-motion (ROM) exercises |
|
Nondisplaced
fracture of the radius or ulna |
Long-arm cast with collar and cuff |
WRIST
|
|
|
Most distal radius fractures without
foreshortening of the radius or with less than 200 of angulation |
Chinese finger-trap
traction plus sugar-tong splint plus short-arm cast |
HAND
|
|
|
Boxer fracture of the fifth metacarpal with less
than 400 of angulation |
Removable volar splint |
|
Volar dislocation
of the MTP with avulsion fracture <2-3mm |
Radial or ulnar gutter splinting |
|
Extra-articular metacarpal fracture of the thumb
without displacement in any plane |
Thumb spica cast plus ROM exercises of the thumb |
|
Dorsal dislocation of the MP joint of the thumb
if a single reduction succeeds |
Dorsal hood splint |
|
Gamekeeper’s thumb,
incompletely ruptured |
Dorsal hood splint |
|
Extra-articular fractures of the proximal and
middle phalanges (nondisplaced and without rotation or angulation) |
Buddy-tape plus ROM exercises |
|
The acute boutonniere injury without avulsion
fracture |
Splinting of the PIP joint in extension plus ROM
exercises of the finger joints |
|
Dislocation of the PIP joint without volar lip
fracture |
Radial or ulnar gutter splinting for 2 weeks,
then buddy-taping |
|
All distal phalanx
fractures |
Stack splint |
|
Most mallet fingers |
Stack splint or dorsal
aluminum splint in full extension |
|
Mallet fractures, displacement <2-3mm |
Stack splint |
CHEST
|
|
|
Rib fracture,
without pulmonary injury |
Wide bra, Ace wrap, or chest binder |
PELVIS
|
|
|
Nondisplaced, nonarticular, with minimal pain |
Touch-down-weightbearing crutches |
HIP
|
|
|
Hip fracture in a debilitated patient |
Prolonged bedrest |
|
Impacted fractures that are weeks old |
Non-weightbearing crutches followed by
touch-down-weightbearing crutches |
|
Stress fractures |
Bedrest vs. crutches vs. reduced running |
|
Avascular necrosis |
Crutches |
KNEE
|
|
|
Patellar, nondisplaced and intact quads |
Long-leg case, well molded at the patella |
|
Avulsion fracture at the joint line |
Velcro straight-leg brace |
|
Osteochondritis
dissecans without mechanical locking or effusion |
Straight-leg raises
and observation |
|
Tibial plateau rim, if <100 |
Long-leg cast |
|
TIBIA |
|
|
All tibial stress
fractures |
No running vs. decreased running schedule |
|
Most minimally displaced tibial fractures, if
<1cm leg shortening or <5-100 of angulation |
Long-leg casting with suprapatellar and medial
tibial molding; neutral ankle position; knee flexed to 50 |
FIBULA, ALL FRACTURES
|
Short-leg walking cast for pain control vs.
reduced standing and walking |
|
GASTROCNEMIUS
TEAR |
No running, reduced standing and walking, tape |
|
ANKLE |
|
|
Isolated small avulsion fractures |
Short-leg walking cast for 2-4 weeks |
|
Nondisplaced single malleolar fractures |
Jones dressing followed by a short-leg walking
cast for 4-6 weeks |
|
Stable bimalleolar fractures |
Jones dressing followed by a short-leg walking cast
for 4-6 weeks. |
|
Posterior process of the talus |
Short-leg walking cast for 4-6 weeks |
|
Lateral process of the talus, nondisplaced |
Short-leg walking cast for 4-6 weeks |
CALCANEUS
|
|
|
Most extra-articular fractures (except the
displaced posterior process fracture) |
Bedrest for 5 days, Jones dressing, short-leg
walking cast with crutches and non-weightbearing, then gradual weightbearing |
TALUS
|
|
|
Chips, avulsions, nondisplaced neck fractures |
Short-leg walking cast for 8-12 weeks |
NAVICULAR
|
|
|
All avulsion, stress, and tuberosity fractures
(except with large fragments) |
Short-leg walking cast for 4-6 weeks |
FOOT
|
|
|
Heel-pad syndrome |
Heel cups or padded insoles |
|
All fifth MTP avulsion fractures |
Short-leg walking cast for 2-4 weeks |
|
Jones fracture of the fifth metatarsal,
nondisplaced |
Jones dressing followed by a short-leg walking
cast for 3-4 weeks |
|
Nondisplaced metatarsal fractures |
Short-leg walking cast with crutches and
non-weightbearing for 2-3 weeks plus casting and weightbearing for an
additional 2 weeks |
|
All stress fractures of the metatarsals |
Well-supported shoe
plus limited standing and walking |
|
Nearly all great toe fractures without
comminution or soft-tissue injury |
Taping plus a well-supported shoe vs. short-leg
walking cast for 2 weeks |
|
Nearly all sesamoid fractures without comminution
or soft-tissue injury |
Short-leg walking cast for 3-4 weeks, then a
well-supported shoe |
|
Lesser toe fractures |
Cotton ball between the toes plus taping |
Fracture Guidelines for Referral to a Surgical Orthopedist
|
Fracture/Dislocation |
Reason for Orthopedic
Referral |
|
All
compound fractures |
Risk
of infection and soft-tissue injury |
|
Nearly all comminuted fractures |
Unstable;
risk of nonunion |
|
Most
intra-articular fractures |
Risk
of arthritis and poor joint function |
|
Most
spiral shaft fractures |
Unstable;
risk of shortening |
|
Most
displaced fractures |
Unstable;
risk of nonunion |
SHOULDER AND UPPER ARM
Clavicle
|
|
|
Associated with rib fracture |
Risk
of lung or great vessel damage |
|
Distal third associated with displacement |
Risk
of nonunion |
|
Humerus |
|
|
Transverse shaft fusion |
Risk
of nonunion |
|
Neck fracture with shoulder dislocation |
Unstable;
risk of arthritis |
|
Fragment
displacement >1cm or angulation >450 |
Unstable |
|
Supracondylar fracture with displacement |
Risk
of arthritis, brachial artery or median nerve injury |
ELBOW AND FOREARM |
|
|
Displaced
radial head fracture |
Unstable |
|
Displaced
fracture of the radius or ulna |
Unstable;
risk of compartment syndrome |
WRIST |
|
|
Displaced
or intra-articular distal radius fracture |
Unstable;
risk of arthritis |
|
Radius
foreshortened by 5mm or angulation >200 |
Risk
of arthritis |
|
Navicular fracture |
Risk
of Avascular necrosis or nonunion |
|
Perilunate
dislocation |
Referral
for primary repair or fusion |
THUMB |
|
|
Gamekeeper’s
thumb, complete tear |
Risk
of poor function |
|
Intra-articular
metacarpal fracture of the thumb—Bennett fracture and Rolando fracture |
Unstable;
risk of arthritis |
|
Dorsal
dislocation of the MP joint of the thumb |
Single
attempt at closed reduction; Sx referral if unsuccessful |
|
Transverse
fracture at the base or neck, spiral oblique, comminuted, and condylar
fracture (intra-articular) |
Unstable;
risk of poor function and abnormal alignment |
|
Fracture/Dislocation |
Reason for Orthopedic
Referral |
HAND |
|
|
Metacarpal
fracture (except the fifth) |
Unstable |
|
Boxer’s
fracture of the fifth MC with angulation >60o |
Unstable;
referral for pin fixation |
|
Volar dislocation of the MCP joints with avulsion fragment >2-3mm |
Unstable;
risk of arthritis |
|
Volar
subluxation of the DIP greater than 2-3mm displacement, or involvement of
>30% of the articular surface |
Referral
for primary repair |
|
Rupture
of the flexor digitorum profundus tendon |
Referral
for primary repair |
PELVIS AND HIP JOINT |
|
|
Pelvic/acetabular
fracture |
Multiple
injuries; unstable; traction |
|
Hip
fracture |
Unstable;
internal fixation |
|
Fracture
of the femur |
Unstable; traction; internal fixation (x infants) |
KNEE
|
|
|
Supracondylar
fracture |
Unstable;
internal fixation |
|
Tibial
plateau depressed >6-8mm |
Unstable;
risk of arthritis; internal fixation |
|
Rim
fracture >10o |
Internal
fixation |
|
Bicondylar fracture |
Skeletal
traction; cast brace; internal fixation |
|
KNEE |
|
|
Tibial
spines |
Molded
long-leg cast for 4-6 weeks |
|
Subcondylar
fracture |
Molded
long-leg cast for 4-6 weeks |
|
Patellar,
displaced or comminuted |
Cerclage
or patellectomy |
|
Osteochondritis
dissecans, symptomatic with locking |
Arthroscopy |
|
Tibial
and fibular fracture |
Unstable;
internal fixation |
ANKLE |
|
|
Unstable
bimalleolar fracture |
Risk
of arthritis; internal fixation |
|
Trimalleolar
fracture |
Risk
of arthritis; internal fixation |
|
Fracture
at or above the syndesmosis |
Unstable;
risk of arthritis |
|
Displaced
ankle fragments |
Unstable;
risk of arthritis |
CALCANEUS |
|
|
Intra-articular
fracture |
Risk
of arthritis |
|
Displaced
posterior process fracture |
Restore
the integrity of the Achilles tendon |
|
Nonunion
of the anterior process |
Internal
fixation |
|
Fracture/Dislocation |
Reason for Orthopedic
Referral |
|
|
|
TALUS |
|
|
Displaced
neck fracture |
Risk
of Avascular necrosis |
NAVICULAR |
|
|
All
displaced fractures |
Unstable |
FOOT |
|
|
Neuropathic
fracture |
Risk
of nonunion or malunion |
|
Transverse
fifth metatarsal fracture |
Risk of nonunion or malunion |
|
Displaced
or comminuted proximal phalangeal fracture |
Risk
of nonunion or malunion |
workshop\fracture.doc\4-12-99